Greetings from the Professor

Welcome to the website of the division of Hematology & Oncology, Department of internal medicine, St. Marianna University School of Medicine. I am Ayako Arai, appointed as the professor of the division as of April 1, 2019. Our department is based on a hill near the Tama river in Miyamae-ku, Kawasaki city. We treat patients with hematologic diseases, educate students and pursue research activities in beautiful natural surroundings full of greenery and blessed with inspirations offered by four seasons.
We are all aware that recent medical advances are remarkable, yet we must admit there are numerous challenges that remain unresolved in the clinical settings. Our goal is to identify solutions to such challenges and deliver them to the patients and the public.
I have specialized in the treatment of hematopoietic tumor and other hematologic diseases using chemotherapy and Hematopoietic Stem Cell Transplantation (HSCT) in my clinical capacity. I also wear a research scientist's hat to analyze the oncogenic mechanisms using a molecular biological methodology. I believe that my mission as a hematology specialist and a medical research scientist is to elucidate the pathogenesis of intractable hematologic diseases and develop a treatment to control them by merging the strengths of clinical medical science and basic medical science. Our team's area of special interest in recent years is to provide care for, elucidate the pathogenesis of, and develop an effective treatment for Chronic Active Epstein-Barr Virus infection (CAEBV) which is classified as an EBV-positive T- or NK-cell neoplasm. It is an intractable disease with hardly any cases reported from the U.S. and western part of Europe. Most cases have been reported from Japan and east Asia to date. We continue to search clues for the following questions: Why does a common virus cause serious diseases in some individuals? Is there any treatment medication to control the disease? Our team is committed to find a cure for all the hematologic diseases including CAEBV.
Our utmost priority is to serve the patients as trusted partners so that they all feel at ease being supported by us. Chemotherapy and transplant which are the standard regimen in the hematology discipline often give a hard time to the patients who are fighting the disease. An interdisciplinary team of physicians, registered nurses, and pharmacists will address their concerns comprehensively so that the treatment is sustainable. We also value QoL (Quality of Life) of the patients. We proactively support patients who receive outpatient chemotherapy and ensure safe and secure treatment. Not only do we brush up our knowledge and skills as technical experts but also hone our human skills so that the patients will have confidence in us.
As we develop undergraduate students and clinical trainees, we help them to become physicians with a heart who can empathize with the patients as they address their needs attentively. Above all I hope to pass on the excitement of studying hematology to them. Our goal is to develop physician scientists who can appropriately extract the essence of the challenge and come to terms with it under any kind of circumstances.
Our class is still small in size and is in a fledgling state. This also means that there is unlimited room for growth. I foresee a series of evidence being launched from the hills of Tama area in Japan to the world.
Ayako Arai MD., PhD.
Professor, Director and Chairperson of the division of Hematology & Oncology, Department of internal medicine, St. Marianna University School of Medicine
How We Provide Care
Care and treatment for hematologic diseases in general is available to both outpatients and inpatients. We try to serve as trusted partners to the patients. A number of experienced care-providing staff support both the outpatient and inpatient care so that patients feel fully informed and feel comfortable to be treated by us.
We participate in JALSG (Japan Adult Leukemia Study Group) to enable ourselves to support the most advanced care for leukemia in Japan. We proactively treat ML (Malignant Lymphoma) and MM (Multiple Myeloma) and participate in clinical trials. Professor Ayako Arai leads the AMED research group that studies Chronic Active Epstein-Barr Virus infection (CAEBV) . Professor Arai is also the principal investigator for the “Phase II Trial investigating the Efficacy and Safety of Ruxolitinib single treatment in patients with CAEBV”, an investigator-initiated study.
https://www.amed.go.jp/news/release_20190109.html
Target Disease
-
Hematopoietic tumor (leukemia, lymphoma, myeloma)
- Chemotherapy
- Hematopoietic stem cell transplantation
- Molecular-targeting therapy (including ZEVALIN®)
- Anemia (aplastic anemia, hereditary hemolytic anemia and acquired autoimmune hemolytic anemia)
- Hemorrhagic Disorder (Thrombocytopenic Purpura, Hemophilia, other hereditary or acquired Coagulation Disorder)
- Chronic Active Epstein-Barr Virus infection (CAEBV)
Number of Outpatient (New Cases)
| FY2015 | FY2016 | FY2017 | FY2018 | FY2019 | FY2020 | FY2021 | |
|---|---|---|---|---|---|---|---|
| Acute Leukemia | 86 (20) | 72 (16) | 63 (15) | 65 (11) | 63 (16) | 52 (13) | 59 (10) |
| Hodgkin Lymphoma | 16 (5) | 19 (3) | 20 (3) | 23 (4) | 16 (1) | 27 (5) | 28 (2) |
| Non-Hodgkin Lymphoma | 450 (53) | 454 (78) | 475 (62) | 485 (60) | 503 (88) | 486 (72) | 506 (76) |
| Myeloma, Amyloidosis | 73 (16) | 75 (16) | 79 (12) | 86 (16) | 98 (16) | 88 (16) | 102 (21) |
| MDS Myelodysplastic Syndrome | 128 (16) | 128 (13) | 115 (5) | 109 (18) | 110 (24) | 88 (23) | 82 (17) |
| Chronic Leukemia | 106 (16) | 100 (6) | 110 (14) | 113 (3) | 110 (8) | 52 (6) | 91 (14) |
| Chronic Active Epstein-Barr Virus Infection (CAEBV) | - | - | 0 | 0 | 2 (2) | 3 (3) | 10 (5) |
| Total | - | - | - | - | 219 | 218 | 185 |
| Cumulative total | - | - | - | - | 306 | 331 | 297 |
Number of Inpatients
| FY2015 | FY2016 | FY2017 | FY2018 | FY2019 | FY2020 | FY2021 | |
|---|---|---|---|---|---|---|---|
| Acute leukemia | - | - | - | - | 60 | 49 | 31 |
| Hodgkin lymphoma | - | - | - | - | 8 | 13 | 2 |
| Non-hodgkin lymphoma | - | - | - | - | 152 | 153 | 171 |
| Myeloma, amyloidosis | - | - | - | - | 21 | 27 | 25 |
| MDS Myelodysplastic syndrome | - | - | - | - | 22 | 16 | 6 |
| Chronic leukemia | - | - | - | - | 2 | 6 | 6 |
| Chronic active Epstein-Barr virus infection (CAEBV) | - | - | - | - | 1 | 6 | 8 |
| Epstein-Barr virus associated diseases | - | - | - | - | 0 | 0 | 0 |
| Myeloproliferative disorder | - | - | - | - | 4 | 4 | 5 |
| Cytopenia | - | - | - | - | 11 | 19 | 10 |
| Other hematologic diseases | - | - | - | - | 2 | 6 | 3 |
| Non-hematologic diseases | - | - | - | - | 20 | 25 | 23 |
| Transplant donor | - | - | - | - | 0 | 6 | 7 |
| Others | - | - | - | - | 3 | 1 | 0 |
| Total | - | - | - | - | 306 | 331 | 297 |
The number of Hematopoietic Stem Cell Transplantation
| FY2016 | FY2017 | FY2018 | FY2019 | FY2020 | FY2021 | ||
|---|---|---|---|---|---|---|---|
| Autologous Transplantation | Peripheral Blood (PB) | 1 | 4 | 2 | 3 | 5 | 2 |
| Allogenic Related Hematopoietic Stem Cell Transplantation | Allogenic Related Hematopoietic Stem Cell Transplantation | 1 | 1 | 0 | 0 | 3 | 4 |
| Allogenic Unrelated Hematopoietic Stem Cell Transplantation | PB | 0 | 0 | 0 | 0 | 0 | 0 |
| Bone Marrow | 0 | 0 | 0 | 0 | 0 | 0 | |
| Umbilical Cord Blood | 0 | 0 | 0 | 0 | 0 | 0 |
Outpatient Shift Timetable of St.Marianna University School of Medicine Hospital
See the home page of each hospital (Japanese only)
Appointments
- St.Marianna University School of Medicine Hospital
- Yokohama City Seibu Hospital
- Kawasaki Municipal Tama Hospital
Second Opinion
For second opinion, choose the hospital for details (Japanese only)
Education
Internship, Post Graduate Medical Education (First Half)
Internship is taught based on the original training program of the St. Marianna University School of Medicine. Medical interns will acquire versatile basic skills (general demeanor, procedures and knowledge) applicable in dealing flexibly and in a holistic manner with the diseases and pathology that are encountered in daily practice as they provide care as interns mainly for the inpatients. Interns will also learn cutting edge medical knowledge and evidence-based basic clinical skills by attending a weekly clinical conference, joint inter-campus conference sessions held 2 times a year.
Click here for more information (Japanese only)
Internship, Post Graduate Medical Education (Second Half)
Interns will be assigned to practice as hematology specialists not only in the St. Marianna University Hospitals but also in the hospitals that are related to the University. Interns will acquire professional skills to provide care and are also given the opportunity to actively publish the findings in professional society meetings and scientific journals. They will also receive necessary trainings to qualify as hematology specialists certified by the Japanese Society of Hematology. Licenses for other specialty that can be acquired in our department are shown below.
Click here for more information (Japanese only)
| Clinical Conference |
General Conference (once a week on Tuesdays from 14:00) The General Conference is followed by the ward round led by the professor. |
|---|---|
| Case Study Conference | Every other Tuesday |
| Clinical and Pathological Conference | Whenever necessary |
| Joint Conference by Yokohama-city Seibu Hospital | The third Thursdays |
| Protocol Conference | Whenever necessary |
| Specialist Licenses and Degrees available in our department | MD, MMSc (Master of Medical Science), Internal Medicine Specialist certified by the Japanese Society of Internal Medicine, General Internal Medicine Specialist certified by the Japanese Society of Internal Medicine, Hematology Specialist certified by the Japanese Society of Hematology, Certified Specialist for Oncology Treatment |
Graduate School, Master's Course, PhD course (physicians, scientists, working professionals are eligible as applicants)
Research
Chronic Active Epstein-Barr Virus Disease (CAEBV)
What We Do
Our department is the only institute in the world that specializes in the care of and the research for Chronic Active Epstein-Barr Virus infection (CAEBV) in adults. CAEBV is a rare disease of two dimensions: systemic inflammation and neoplastic disease.
The former dimension is characterized by chronic inflammatory symptoms (fever, lymphadenoma, liver dysfunction, vasculitis, and neurological findings) and the latter is characterized by the malignant proliferation of EB virus-infected T- or NK cells identified in the peripheral blood of the patients. Most cases are reported from Japan and other parts of East Asia. Very few cases are reported from the Western world. Initially it was reported that it is a pediatric disorder or disorder frequent among the young adults. But as CAEBV draws more attention, the number of adult cases reported is increasing in recent years. We believe that the Japanese researchers have the obligation to develop a solution for this disease and share the information with the global community of practitioners. Professor Ayako Arai, the group leader, is addressing the challenges of CAEBV as the Principal Investigator of “Phase II Trial to investigate the Efficacy and Safety of JAK1/2 Inhibitor Ruxolitinib in Patients with CAEBV Infection”, an investigator-initiated study funded by the Practical Research Project for Rare/Intractable Diseases at AMED (Japan Agency for Medical Research and Development).
She also participates as a co-researcher in the “Building of the Disease Registry and Biobank of Chronic Active EB Virus Infection and Relative Diseases”, an intractable disease policy research project hosted by the Japanese Ministry of Health, Labor and Welfare. She plays a role in developing guidelines for the treatment and disease registry. She is also engaged in patient advocacy through CAEBV patient organization SHAKE (http://caebv.com/).
In Pursuit of a Better Care
EBV infected T- or NK cells must be identified first to diagnose a patient with CAEBV. This is why it is difficult to identify the disease by general examination. Besides, an effective regimen has not been established yet. A quick and accurate diagnosis method, elucidation of pathogenesis and the development of an effective treatment is urgently required. Our department strives jointly with National Health Center for Child Health and Development and Tokyo Medical and Dental University to provide quick and accurate diagnosis.
In order to elucidate the mechanisms of the disease
We are currently trying to elucidate the pathogenesis of the CAEBV infection and are developing new treatments with the grant extended by AMED (Japan Agency for Medical Research and Development) as part of the basic research efforts. We have been successful in developing the disease model mouse, and clarified the molecular mechanisms of immortalization process and malignant transformation of the EBV-associated T-or NK cells.
We also published a paper on retrospective analysis of the pathogenesis of adult cases in Japan and the outcome of hematopoietic stem cell transplant cases. Details can be found in the research track record of our department. We also started the investigator-initiated study investigating the efficacy and safety of Ruxolitinib in 2019.
Our Mission
CAEBV infection is a serious disease. As there is not any patient in Europe and in the USA, Japanese researchers are obligated to elucidate its pathogenesis. We would like to make use of all the information provided by the patients to develop an efficacious treatment.
Prognosis Factors in ML
Outline
The theme of my research is the analysis of prognosis factors in malignant lymphoma, the most frequent tumor in hematology. I have spent time especially focusing on the risk of central nervous system (CNS) invasion in diffuse large B-cell lymphoma (DLBCL). Among the journals and the reviews I have published, I recently reported that International Prognostic Index (IPI), one of the typical prognostic factors of DLBCL, can be used to evaluate the risk of CNS invasion (Figure 1). I plan to investigate various gene mutations to explore possible risk of CNS invasion.
Lymphoma characterized by the rearrangements of both Myc gene and BCL2 gene is called double-hit lymphoma (DHL). I reported that the prognosis of DHL is poor (Figure 2), and I believe that this report became a prototype of DHL research which is now common world-wide. I am proud and honored that my review article published at the time was cited by the WHO classification 2017. In 2013, I was awarded Yokohama University City Medical Association Award for these studies.
I am fully committed to continue my research and widely communicate on the prognosis improvements of malignant lymphoma.
(Figure 1. Leukemia and Lymphoma 2018)
(Figure 2. Haematologica 2009)
New Therapy for MLL
Research Area
The development of new therapy for mixed-lineage leukemia (MLL)
Outline
MLL is a general name of leukemia with an MLL gene abnormality at chromosome 11q23. The age of patients varies from infants to adults. The prognosis is commonly known to be poor, and it is rarely cured even with a multimodal therapy. I am striving to develop a new therapy, which is earnestly desired.
Research by a Clinician
I decided to become a doctor when my friend passed away before entering elementary school. As a result of my persistence, fortunately or unfortunately, I became a hematologist especially interested in hematopoietic stem cell transplantation (HSCT). HSCT is sometimes praised as a dream therapy but the reality is not necessary a dream. It may save a patient from a critical condition, but it may be a cause of a patient loss due to severe complications from the treatment, or it may result in a relapse after a condition which appeared as a complete cure. One can describe HSCT as a treatment of heaven and hell. While I devoted myself in this treatment, I encountered a disease called "mixed-lineage leukemia", known as MLL. The age of patients varies from infants to adults, and the prognosis is commonly poor. It is rarely cured by a multimodal therapy. As a resident physician, I looked after two MLL patients. Both patients successfully underwent HSCT during the first remission phase and maintained remission over a year. However, relapse occurred in both cases. This was a shocking experience and at the same time intuitively made me convinced that the disease has a mechanism to escape from the effect of HSCT. This conviction turned into my mission, which is to formalize my intuition and overcome MLL.
Today's Achievements
Our team developed MLL model mice from MLL patient genes (Figure 1). In the analysis, we discovered that MLL escapes from the graft-versus-leukemia (GVL) effect through the expression of S100A6, a calcium binding protein. GVL is an efficacy of donor-originating immune cells to attack residual recipent-originating leukemia, and it is an important effect after the transplantation. This discovery was the formalization of my intuition (Figure 2). At last, we succeeded in model mice to cure MLL by blocking this mechanism of S100A6 mediation to escape from GVL effect. We presented the outcome of the study at the American Society of Hematology (ASH) and the European Hematology Association (EHA) meetings. The study was finally published as a journal on different media (References 1-4).
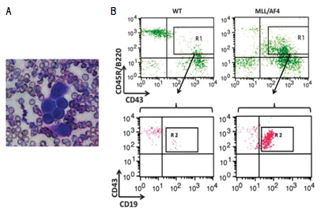
Figure 1. Our MLL/AF4 transgenic model mice develop acute lymphoblastic leukemia (ALL) after 12 months from birth.
A. ALL in peripheral blood, B. Surface marker of peripheral blood cells
(Modified figure from reference 1)
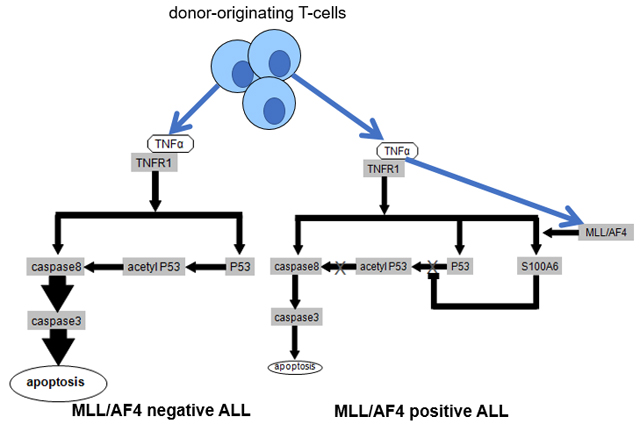
Figure 2.
(Modified figure from reference 3)
Left: Working hypothesis of the effect of TNF-α on MLL/AF4 negative ALL. TNF-α seems to lead leukemia cells to apoptosis through caspase 8–caspase 3 pathway or p53–caspase 8–caspase 3 pathway.
Right: Working hypothesis of the pathway of MLL/AF4 positive ALL to be resistant to TNF-α. MLL/AF4 positive ALL seem to be resistant to TNF-α by upregulation of S100A6 via inhibition of upregulation of the p53–caspase 8–caspase 3 pathway.
Next Step: Returning the Research Achievements Back to Clinical Practice
It is my dream to return the achievements from these studies back to clinical treatment of MLL patients. To make this treatment more available, we went through many trials and errors to look for an existing drug to suppress S100A6. We finally discovered the possibility of amlexanox, an anti-allergic drug, to block S100A6 from mediating GVL-effect-escape. Our study was adopted and published (Reference 5). I will continue my research as a clinician to apply the study findings in practice of treating MLL.
- 1: Tamai H, et al. Activated K-Ras protein accelerates human MLL/AF4-induced leukemo-lymphomogenicity in a transgenic mouse model. Leukemia. 2011;25: 888-91.
- 2: Tamai H, et al. AAV8 vector expressing IL24 efficiently suppresses tumor growth mediated byspecific mechanisms in MLL/AF4-positive ALL model mice. Blood. 2012;119: 64-71.
- 3: Tamai H, et.al. Resistance of MLL-AFF1-positive acute lymphoblastic leukemia to tumor necrosis factor-alpha is mediated by S100A6 upregulation. Blood Cancer J. 2011;1: e38. doi: 10.1038/ bcj.2011.37.
- 4: Tamai H, et al. Inhibition of S100A6 induces GVL effects in MLL/AF4-positive ALL in human PBMC-SCID mice. Bone Marrow Transplant. 2014;49: 699-703.
- 5: Tamai H, et.al. Amlexanox Downregulates S100A6 to Sensitize KMT2A/AFF1-Positive Acute Lymphoblastic Leukemia to TNFα Treatment. CancerRes.2017;77:4426-4433.
Achievements
(Japanese Only) FY: April-March
Our Team
-
Professor, Head of the Department
Ayako Arai
Personal Profile -
Professor
Naoto Tomita
Current Research -
Professor
Hayato Tamai
researchmap
Current Research -
Specially Appointed Professor
Toshiki Watanabe
researchmap -
Specially Appointed Professor
Fumiaki Sano -

Specially Appointed Professor
Hiroshi Yasui
researchmap -

Associate Professor
Kumi Oshima -

Specially Appointed Associate Professor
Masayuki Kato -

Assistant Professor
Yoshinori Suzuki -

Assistant Professor
Sanshiro Uchida -

Assistant Professor without Tenure
Aika Fuseya -

Assistant Professor without Tenure
Subaru Wakisaka -

Part-time Lecturer, Registered Medical Practitioner of Yokohama City Seibu Hospital
Madoka Takimoto -

Part-time Lecturer
Kota Ohashi -

Part-time Lecturer
Masatoshi Kanno
researchmap -
Registered Medical Practitioner
Kentaro Matsuura -
Registered Medical Practitioner
Hanae Shimura -
Hematopoietic Cell Transplant Coordinator
Akane Hosokai
- Research Technician
- Junko Asano
- Department Secretary
- Natsuko Habuka
- Assistant to Professor Ayako Arai
- Ayako Komoto
Yokohama City Seibu Hospital
-

Professor
Akihiro Yokoyama
researchmap
Kawasaki Municipal Tama Hospital
-

Senior Lecturer
Yu Uemura
Career and Residency
If you are a physician or a scientist who wants to find solutions to turn blood disorders to curable diseases, join our team full of experiences and talents! We strive to offer challenges to meet different career goals.
- I want to gain proficiencies and skills as a hematology physician.
- I want to be a certified hematologist of the Japanese Society of Hematology
- I want to study as a graduate student
- I want to study as a postdoctoral researcher
- I want to work as a hematology physician balancing time between work and family
- I want to return to work after a maternity leave or any other long leave
Don't worry even if you don't specialize in hematology now. As long as you are interested in blood disorders, you can be part of our team. On top of your current expertise, add the knowledge and experiences in hematology with us.
If you wish to work part-time, for instance a few days a week or only on duty, please consult with us. Let's work out what works best for you. Start your career with us now!
Ayako Arai
Professor
Residency at Hematology and Oncology, St Marianna University School of Medicine
We are proud to be competitive in the following areas:
- Number of cases
- Number of training institutions
- Variety of experienced trainers
- Variety of trainers' backgrounds
- Variety of options after residencies
We partner with not only our group hospitals but also with National Cancer Center Japan, Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital, and many other renowned institutions.
Start your journey of hematology with us.
Ayako Arai
Professor
You may not be confident in your knowledge or skills when you start your career, but confidence can always be built by effort, education, and your learning environment. Beyond physicians' knowledge is building trust with patients.
Having knowledge and practicing medicine does not automatically result in gaining trust from patients. First, we must understand patients' social background such as their family and economical situation. In planning treatment strategies, we must respect patients' preferences as much as possible. We must pay respect not only to patients' educational background, career, family, and life history but also to their families and those who support them. Because many of our patients must put their lives on the line to our treatments, we have opportunities to gain patients' trust. Actually, it is our mission to be trusted. I hope that young doctors acquire such skills in the process of building experiences and that we give patients energy for life.
Masayuki Kato
Specially Appointed Associate Professor
Our hospital functions not only as a main hospital in the area but also as a university hospital. While we treat hypoferric anemia, we conduct allogeneic hematopoietic stem cell transplantation and clinical research, which requires highly advanced technology and facility. You can learn the different aspects and clinical activities of hematology.
In Europe, a hematology physician is called “the king of physicians” because we are involved from the start until the end, from diagnosis to treatment. Experience the dynamic tasks and missions to fight against diseases together with our patients.
Yasuyuki Inoue
Associate Professor
Department of Hematology
Yokohama City Seibu Hospital
For inquiries and application for jobs or residencies, contact
Ayako Arai
Professor
Division of Hematology and Oncology
Department of Internal Medicine
St. Marianna University School of Medicine
2-16-1 Sugao
Miyamae-Ku, Kawasaki 216-8511
Phone: +81-44-977-8111, ex. 3372
E-mail: ara.hema@marianna-u.ac.jp